The Power of Light
A corona mass ejection erupts from our sun on August 31, 2012 - photo provided by NASA.
THE POWER OF LIGHT
“We can easily forgive a child who is afraid of the dark; the real tragedy of life is when men are afraid of the light.” -PlatoCurrently, it is estimated that over 1 billion people worldwide are vitamin D deficient, largely due to our modern avoidance of the sun. Other scientists have have labeled vitamin D deficiency a pandemic, while more have argued that the number of deficient individuals could actually include up to 50% of the world’s population. For many years, scientific inquiry has focused on the health risks of sun exposure, especially skin cancers, while the risks of inadequate sunlight have gone largely ignored. However, because of the major role vitamin D and light plays in optimizing your health, it’s important to understand how light affects our biology and how you can adjust your lifestyle to safely maximize your light exposure.
Let’s start with the basics: What is light? Light is all around us. Known as electromagnetic radiation (EMR) or the electromagnetic field, light is made up of varying waves of elementary particles called photons. Photons are massless, stable, and have no electrical charge. The energy and momentum of a photon depend only on its wavelength and frequency. The light spectrum is composed of the variation of different wavelengths or frequencies that are produced by a light source. The visible light spectrum ranges from 380 nm to 780 nm, but the entire spectrum includes gamma rays, x-rays, ultraviolet (UV) rays, infrared rays (IR), radar, FM, TV, shortwave, and AM. Essentially, visible light is a small section of the electromagnetic spectrum, which is the complete range of possible frequencies of electromagnetic radiation and photon energies. The frequency or wavelength of visible light is often perceived by colors, notably blue, red, yellow, and green, but there are many other shorter or longer wavelengths that are invisible to the human eye.
What happens when light comes into contact with matter? Matter is composed of atoms, ions, and molecules. Atoms and molecules contain electrons, which tend to vibrate at certain frequencies due to their electrical charge. When a light wave is enacted on an atom or “absorbed”, the electron begins to vibrate in accord with that same electromagnetic frequency (called wave oscillations). It’s like tuning a musical instrument. The neighboring atoms around our initial atom then begin to vibrate or oscillate as well, creating thermal energy, or heat.
Light frequencies travel and can enter the body through two primary entry points: the retina and the skin. Absorption of light into the human body is ultimately a reduction in energy, but it also plays a pivotal role in how your body functions. Throughout all of human history (arguably until very recently) our main source of light has been from the sun and our biology is not only tuned to its frequencies, but we’ve evolved to depend on it.
Check out this helpful video for a deeper dive and visuals of the electromagnetic spectrum:
Skin in the Game
Figure 1. from Vitamin D: The “Sunshine” Vitamin
Unlike other essential vitamins, which are obtained from food, vitamin D3 is mostly synthesized in the skin through a photosynthetic reaction triggered by exposure to the sun’s radiation, particularly from ultraviolet B rays (UVB, between 290–315 nm). 7-dehydrocholesterol is a cholesterol precursor that is found in the epidermal layer of skin. When UVB rays hit the skin, 7-dehydrocholesterol is converted into previtamin D3 as a mechanism to absorb this electromagnetic energy. After sun exposure only about 15% of 7-dehydrocholesterol can convert to previtamin D3, thus making it impossible to overdose on vitamin D3 from sun exposure. The rest converts to lumisterol3, tachysterol3, or reverts back to 7-dehydrocholesterol. Previtamin D3 then enters the bloodstream on a plasma binding protein and goes through two different hydroxylations (an oxidative reaction) in the liver and the kidneys in order to become an active form of vitamin D3 (25-hydroxyvitamin D, the major circulating form of vitamin D3). However, most cells and organs in the body also have a vitamin D receptor (VDR) and many cells and organs are able to produce a bioactive version of vitamin D3 (1,25-dihydroxyvitamin D) as well, including the skin itself. Most of the vitamin D3 that is produced in the skin is made in the epidermis and then remains in the skin even when the skin is washed with soap and water immediately after the exposure to sunlight.
When ultraviolet A rays (UVA, 315 nm to 400 nm) hit the skin, it triggers the production of nitric oxide (NO). Having optimized levels of NO carries many therapeutic benefits, such as reducing blood pressure, but more importantly it acts as a potent vasodilator, meaning that it opens (or dilates) blood vessels. More open and pliable blood vessels, means better transportation of vitamin D, previtamin D and its metabolites throughout the body. Paradoxically, having optimized levels of vitamin D also stimulates more NO production in the skin. So you need sun exposure to produce NO, in order to help carry previtamin D through the bloodstream to produce active vitamin D3, which then stimulates the production of more NO in the skin. But NO may also plays an even more intricate role in the delicate balance of light absorption. UV light does not pass through more than a millimeter of skin, so in order to actually absorb and utilize UV light, the circulatory system has to go to it. NO rushes into the dermal layer in order for your hemoglobin to access both UV and infrared (IR) light waves. This vasodilation results in a reddish appearance on your skin. There is a also a sensitivity scale to the process, meaning that if you live in a northern latitude and spend 3/4 of your year indoors, then when you go outside in the summer an acute toxic reaction is more likely to occur, namely prostaglandins and cytokines being recruited during the dilation of these blood vessels.n Conversely, if you live closer to the equator and/or spend more time outdoors, you may have built up more of a resistance to this process.
Melanin, Latitude, & Altitude
Robby at the Equator in rural Uganda.
Only roughly 1% of UVB radiation from the sun ever reaches the earth’s surface – even in the summer at noon – because most of it is absorbed by the stratospheric ozone layer. But the ozone layer isn’t nature’s only protection from the sun’s radiation. Melanin plays a major role in vitamin D absorption by providing a mechanism in your skin to absorb radiation in the spectrum of 290–700 nms. All humans have the same number of melanocytes in their skin, which is a melanin-forming cell, but some people produce more melanin than others depending on where their recent ancestors lived on the planet. Melanin is produced in specific ovoid organelles known as melanosomes, which are produced in dendritic melanocytes that account for only 1% of epidermal cells. Melanin is then transported to adjacent keratinocytes, and accumulate within keratinocytes and melanocytes in the perinuclear area as supranuclear “caps” that are thought to shield DNA from UV rays, the composition of which is dependent on how much protection you need from the sun. The first humans evolved in equatorial Africa, where the direct angle of sunlight delivers the strongest ultraviolet rays. They didn’t have clothing, houses, sunscreens, sunglasses, contacts, or any other modern convenience that inhibits sun exposure. They had skin in the game, quite literally absorbing the maximum amount of sunlight each day and their biology evolved to meet those conditions. But as some humans migrated further away from the equator, they needed to produce less melanin in order to increase light exposure. So in order to survive, be strong, healthy, and able to procreate, skin pigmentation had to decrease in order to permit more UVB photons to enter the skin. Fairer skin complexions are an evolutionary response to migration from the equator, or in other words, it is nature’s solution to allow the optimal vitamin D production to occur at different latitudes. This means that fairer skin requires less time in the sun to reach optimal vitamin D levels. It is well-documented that latitude still continues to play a vital role in vitamin D absorption, especially as people with more melanin in their skin have migrated to latitudes farther from the equator in the modern era. Since melanin inhibits sun absorption, and subsequently, vitamin D production, it can potentially lead to a host of health complications for people with more melanin that live in non-tropical climates, like North America or the United Kingdom. The more melanin produced by melanocytes in your skin, combined with a further distance from the equator, directly correlates to the amount of time that you need to spend in the sun in order to optimize your vitamin D levels.
Figure 1 from The Protective Role of Melanin Against UV Damage in Human Skin
Melanin Content in Skin of Different Ethnicity: Histological detection of melanin content using Fontana-Masson staining. Melanin content in the basal layers of the epidermis is substantially higher in Black skin compared to Asian or White skin, although the number of melanocytes is virtually identical in skins of different ethnicity.
The further you move from the equator, the more cases of high blood pressure, heart disease, stroke, and overall mortality you will find. Dr. Richard Weller, a dermatologist at the University of Edinburgh elaborates on this correlation between sunlight and blood pressure:
“Sure enough, when he exposed volunteers to the equivalent of 30 minutes of summer sunlight without sunscreen, their nitric oxide levels went up and their blood pressure went down. Because of its connection to heart disease and strokes, blood pressure is the leading cause of premature death and disease in the world, and the reduction was of a magnitude large enough to prevent millions of deaths on a global level."
Now, latitude and melanin are the not the only factors that influence the amount of UV radiation that you are able to get from the sun. You live in a 3D plan, so not only do you exist within a certain latitude and longitude, but you also inhabit a specific altitude. The higher the altitude, the shorter the distance that UVB has to travel from the sun to you and thus the skin can produce more vitamin D3. This has been demonstrated with experiments run at Agra (169 M altitude), Katmandu (1400 M), and Mount Everest base camp (5300 M).
Similarly, the earth has seasons due to its axis tilt, which alters the distance from the sun as the earth orbits. Because of this, vitamin D levels typically drop during the colder months of the year (coupled with people covering their skin with more clothing to stay warm). This is vitally important as each hemisphere approaches the cold season because sunlight also regulates serotonin production, which is why people that live further from the equator are more likely to experience “seasonal affective disorder” and have poorer overall health outcomes in the colder months.
The Clinical Benefits of Vitamin D
Often called the “sunshine vitamin,” vitamin D is actually a fat-soluble steroid hormone that regulates the expression of more than 1,000 genes in the body, critically impacting the immune system, as well as the circadian system through structures in the brain. It is also a vital nutrient for calcium absorption, critically affecting skeletal health, as well cardiovascular health.
Outlined above, the biological process which creates this hormone is complex. As sunlight hits the skin, it is incorporated into chylomicrons and absorbed into the bloodstream via the lymphatic system. It then requires hydroxylations in the liver and then even further hydroxylation in the kidneys in order to create the most bioactive form of vitamin D. This process also stimulates calcium absorption in the intestines. Without proper vitamin D levels, only 10-15% of calcium needed can ever be absorbed from our food.
In their literature review, Vitamin D: The “Sunshine” Vitamin, researchers Rathish Nair and Arun Maseeh note that the “vitamin D receptor (VDR) is present in most tissues and cells in the body. [VDR] has a wide range of biological actions, such as inhibition of cellular proliferation and inducing terminal differentiation, inhibiting angiogenesis, stimulating insulin production, inhibiting renin production, and stimulating macrophage cathelicidin production.” Those biological processes include the affect that sunlight has in enhancing the energy production of mitochondria, which is commonly known as “the powerhouse of the cell.”
Dr. Zahid Naeem also recognizes that vitamin D deficiency is a global health crisis. He notes that vitamin D deficiency has been shown to lead to obesity, diabetes, hypertension, depression, fibromyalgia, chronic fatigue syndrome, osteoporosis and neurodegenerative diseases including Alzheimer’s disease. According to Naeem, “Current research [even] indicates vitamin D deficiency plays a role in causing seventeen varieties of different cancers as well as heart disease, stroke, autoimmune diseases, birth defects, and periodontal disease.”
A 2014 observational study in Sweden assessed women that avoided of sun exposure as a risk factor for all-cause mortality. The study followed 29,518 Swedish women for 20 years and found that sun avoidant behavior actually increased risk of all-cause death with a twofold increased mortality rate compared to those with the highest sun exposures. Shockingly, this study also found that lifelong smokers in the highest sun exposure group were at a similar risk as non-smokers avoiding sun exposure, which indicates that avoiding the sun can carry the same magnitude of risk to your overall health as smoking cigarettes.
Cancer
A PubMed database search yielded 63 observational epidemiological studies of vitamin D in relation to risk of cancer, including 30 of colon, 13 of breast, 26 of prostate, and 7 of ovarian cancer, and several that assessed the association of vitamin D receptor genotype with cancer risk found that the majority of studies found a protective relationship between sufficient vitamin D status and lower risk of cancer. Vitamin D decreases cell proliferation, increases cell differentiation, stops the growth of new blood vessels, and has very strong anti-inflammatory effects. Adequate UVB exposure has even been shown to reduce the risk of prostate cancer. Previous research has suggested a strong link between low vitamin D levels and an increased risk of cancer, with the strongest evidence being for risk of colorectal cancer. There is also evidence linking higher vitamin D intake to a lower risk for breast cancer. Although a definitive connection has not yet been reached between the association of vitamin D and cancer, most evidence seems to point to low vitamin D levels increasing risk of cancer development.
Heart Disease
Vitamin D deficiency has been associated with risk of cardiovascular disease. Research has suggested that the protective effect of vitamin D on the heart could be through the renin–angiotensin hormone system, through the suppression of inflammation, or by directly affecting the cells of the heart and blood-vessel walls. In the Framingham Heart Study, patients with low vitamin D levels had a 60% higher risk of heart disease than those with adequate levels. Other studies have shown that vitamin D deficiency could lead to a 2-fold increase in rates of myocardial infarction. Another study, which followed men and women for 4 years, found that patients with low vitamin D levels were three times more likely to be diagnosed with hypertension than those with adequate levels. The third National Health and Nutrition Examination Survey (NHANES-III) showed that healthy blood pressure and pulse pressure were significantly correlated with vitamin D levels among 12,644 participants. This evidence was corroborated in studies examining the relationship between age, blood pressure, and vitamin D.
Obesity
Vitamin D deficiency is strongly correlated with obesity and some researchers have proposed that it may even provide a causal mechanism. Low levels of vitamin D have been associated with poor BMI, waist circumference, and body fat, whereas adequate levels have been associated with decrease biological age and lean body mass. Low vitamin D levels have also been associated with higher adipose tissue and lower HDL, particularly in individuals with higher amounts of melanin in their skin and living at latitudes farther from the equator. Weight loss has also been associated with an increase in vitamin D levels among postmenopausal overweight or obese women. Low vitamin D has been strongly associated with various types of metabolic illness such as obesity, diabetes mellitus, insulin resistance, cardiovascular diseases including hypertension.
Diabetes
Vitamin D levels have been shown to be lower in individuals with diabetes mellitus type 2 than in control groups. Other research appears to show that vitamin D deficiency may even be causal to the development of diabetes mellitus type 2 and not simply correlational, with individuals that have adequate vitamin D levels notably having a decreased risk of disease development (see Pittas et al. 2007, 2010, 2012; Mitri et al. 2011; Chagas et al. 2012, Lim et al. 2013). Vitamin D also seems to affect glucose homeostasis and has been found to be inversely related to glycosylated hemoglobin levels in gestational diabetes mellitus.
It’s also worth noting that blue light, such as the light emitted from most electrical devices that we use in the modern era, has been shown to impair glucose tolerance and increase sugar intake. This research suggests that not only could vitamin D deficiency due to lack of sun exposure potentially be a causal component of diabetes, but that negative light exposure from modern devices could be aiding in that disease pathophysiology.
Depression
A Norwegian randomized double blind trial of overweight subjects showed that those receiving a high dose supplementation of vitamin D (20,000 or 40,000 IU weekly) had a significant improvements in symptoms of depression compared to the group receiving a placebo supplement. The results of this study further suggest a strong a correlation between vitamin D and the risk of depression. Vitamin D is also a neuroactive steroid and can increase amounts of dopamine, tyrosine, and serotonin in the brain — all of which can help to improve overall mood. A meta-analyses revealed that bright light therapy and sun exposure was associated with a significant decrease in depression symptoms and was an effective intervention for both seasonal affective disorders, as well as nonseasonal depression. Other studies have confirmed a dose-response relationship between sunlight exposure and overall mood, meaning that increases in sunlight exposure simultaneously improved mood.
Cognitive Impairment
An Italian population-based study in Chianti (InCHIANTI) showed that low levels of vitamin D were associated with substantial cognitive decline in the elderly population over the investigative duration of 6 years. The results from this study also suggest that low levels of vitamin D may be especially detrimental to executive functioning, whereas memory and other cognitive domains may be less at risk. The sun can also increase orexin (hypocretin), which is a neuropeptide that helps to regulate several homeostatic functions including the sleep/wake cycle, food intake, energy homeostasis, and arousal. There also seems to be a direct correlation between sun exposure (studied seasonally) with concentrations of Brain-Derived Neurotrophic Factor (BDNF), which is the brain’s key molecule involved in plasticity relating to learning and memory. Low levels of vitamin D have also been strongly indicated as a risk factor for dementia and Alzheimer’s disease. Other research has shown that vitamin D may even be neuro-protective against developing multiple sclerosis (MS) and other neurological disorders.
Alzheimer’s Disease
A 2014 study took a group of 1,658 Americans age 65 and older who were able to walk unaided and who were free of dementia and then performed a followed up check on them in 6 years. Shockingly, the investigators found that participants with a vitamin D level below 10 ng/mL were twice as likely to have developed Alzheimer’s disease during that six year period.
Parkinson’s Disease
Recently, it has been suggested that chronic vitamin D deficiency may play a significant role in the development of Parkinson's disease. A cohort study based on the Mini-Finland Health Survey demonstrated that low vitamin D levels may even predict the onset of Parkinson's disease. Other studies have examined how adequate vitamin D levels may help to decrease the risk of Parkinson’s disease.
Psoriasis
A 2012 study found that patients with psoriasis were more likely to also have low levels of vitamin D. The investigators noted that sun exposure and vitamin D derivatives are commonly used to treat psoriasis.
Pregnancy
Obstetic endocrinology has amassed a wide array of literature all pointing to the importance of vitamin D in pregnancy. Vitamin D requirements in pregnancy women are greater than in the normal population, particularly during the third trimester. Poor levels of vitamin D during pregnancy have been linked to a variety of disordered manifestations in infants, including rickets, osteomalacia, bone disorders, metabolic disorders, as well as other deficiencies for the child in development. Low vitamin D risks for the mother include pregnancy – induced hypertension, high blood pressure in diabetic pregnancy, gestational diabetes mellitus, recurrent pregnancy loss, preterm delivery, primary Caesarian section, and postpartum depression. An analysis of data from the National Health and Nutrition Examination Survey showed that in pregnant women, low levels of vitamin D were associated with nearly a 3-fold increased risk for Bacterial Vaginosis (BV).
Bone Fractures and Falls
Vitamin D is known to play a significant role in bone health by helping the body to absorb calcium. It has also been theorized that vitamin D may increase muscle strength, particularly through receptors on fast-twitch muscles, thereby preventing falls. A combined analysis of 12 fracture-prevention trials found that supplementation with about 800 IU of vitamin D per day reduced hip and nonspinal fractures by about 20%. Additionally, researchers at the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University have examined trials of vitamin D versus placebo for falls, concluding that “fall risk reduction begins at 700 IU and increases progressively with higher doses.”
Autoimmune Diseases
Due to vitamin D’s various immunomodulatory, anti-inflammatory, antioxidant and anti-fibrotic actions, many researchers have been investigating how it may play a role in the pathophysiology of autoimmune diseases. In a 2019 literature review of more than 130 studies, researchers found that low vitamin D levels were directly associated with several autoimmune diseases, such as SLE, thyrotoxicosis, type 1 DM, MS, iridocyclitis, Crohn’s disease, ulcerative colitis, psoriasis vulgaris, seropositive RA, and polymyalgia rheumatica.
Liver Disease
A 2015 review showed that sun exposure has the potential to curtail the development of non-alcoholic fatty liver disease (NAFLD) and found an inverse association between the two, suggesting that sunlight can effectively prevent liver inflammation.
Influenza
Researchers have theorized that vitamin D deficiency may be the seasonal stimulus that triggers influenza outbreaks in the winter. In a randomized, controlled trial, Japanese children were given a daily vitamin D supplement of 1200 IU and subsequently had a 40% lower rate of influenza type A compared with those given placebo.
Pelvic Floor Disorders
The frequency of Pelvic floor disorders is rapidly increasing with age, including urinary and fecal incontinence. Pelvic floor disorders have been linked to osteoporosis and low bone mineral density and remain one of the most common reasons for gynaecologic surgery today. Subnormal levels of vitamin D are common among women, and a such, lower levels are associated with a higher likelihood of pelvic floor disorders according to an analysis of the National Health and Nutrition Examination Survey. Results from the same survey confirmed that lower vitamin D levels are associated with a greater risk for urinary incontinence in women over 50 years old.
Statin intolerance
A 2015 study found that statin intolerance due to myalgia, myositis, myopathy, or myonecrosis can be effectively resolved with vitamin D supplementation. The author’s noted that sun exposure could have a role to play in treating vitamin D deficiency in these patients.
Macular Degeneration
Optimized levels of vitamin D appear to be associated with a decreased risk for the development of early age-related macular degeneration (AMD) among women younger than 75 years old.
Aging
Research has indicated that a vitamin D deficiency can accelerate aging and age-related disease, by promoting autophagy, decreasing inflammation, optimizing mitochondria, decreasing oxidative stress, enhancing Ca2+ in the brain, promoting a positive epigenetic expression, and helping to maintain telomere length. Other studies have confirmed that vitamin D deficiency plays a pivotal role in mitochondrial dysfunction, which has be associated with premature aging. One other study conducted on over 2,000 women found that low levels of vitamin D were associated with shorter telomeres, whereas optimal levels of vitamin D were associated with longer telomeres. Telomere length is a well-known biomarker for biological age, with longer telomere length reflecting a younger age.
Tooth Decay
Vitamin D deficiency is associated with higher rates of periodontitis and gingival inflammation, tooth decay, caries, and a wide array of oral health disorders.
All-cause mortality
A 2014 meta-analysis of data from 73 cohort studies with 849,000 participants and 22 randomized controlled trials with 31,000 participants found that decreased vitamin D levels increased risk for cardiovascular diseases, cancer and other causes (RR 1.35, 95% CI 1.22–1.49 for all cause mortality, comparing the bottom third versus top 2-thirds of baseline circulating 25(OH)D distribution). The authors of this analysis noted that 9.4% of all deaths in Europe and 12.8% in the United States could be directly attributed to vitamin D insufficiency.
Another 2016 meta-analysis pooled the data from 32 studies (30 cohort studies and 2 nested case-control studies) that examined age-adjusted all-cause mortality and vitamin D levels and found that individuals in the group with the lowest levels of vitamin D had nearly twice the death rate of the group with the highest levels of vitamin D.
A 2014 study that followed 29,518 Swedish women in a prospective 20-year follow-up of the Melanoma In Southern Sweden found that habitually avoiding the sun increased risk of all-cause mortality by 40%.
Vitamin D & the Immune System
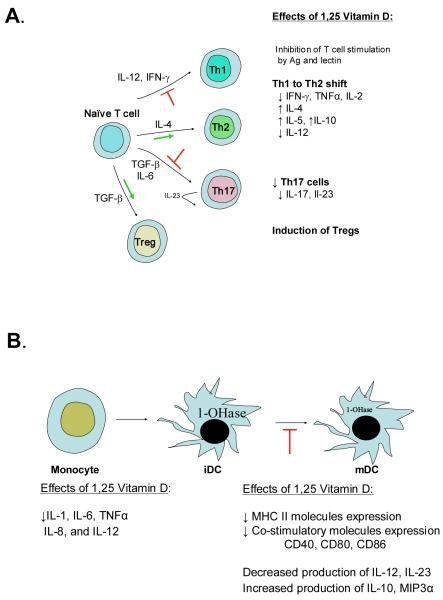
Figure 1 from Vitamin D and the Immune System
A. Effects of 1,25 Vitamin D on T cells include suppression of T cell proliferation, a shift from Th1 to a Th2 development, inhibition of Th17 cell development and facilitation of T regulatory cells. B. Effects of 1,25 Vitamin D on monocytes and dendric cells include inhibition of inflammatory cytokine production by monocytes and inhibition of dendritic cell differentiation and maturation.
Increasing evidence suggests that vitamin D may be a primary modulator of the immune system. Heliotherapy was previously used to treat infections such as tuberculosis before the advent of effective antibiotics, suggesting that vitamin D is a key player in how the immune system responds to threats. Tuberculosis patients were sent to sanatoriums to received heliotherapy, which at the time was thought to directly “kill the tuberculosis.,” although now we understand more of the biological mechanisms that underpin this. There have been many cross-sectional studies associating low levels of vitamin D with increased risk of infection. One such study followed almost 19,000 subjects between 1988 and 1994 and found that individuals with lower vitamin D levels were more likely to develop an upper respiratory tract infection than those with sufficient levels, even after adjusting for potentially confounding variables including season, age, gender, body mass and race. Other studies have made the same correlation between vitamin D and influenza, bacterial vaginosis, and even HIV. Although the exact mechanisms by which light modulates the immune system are still unclear, it appears that T lymphocytes possess an intrinsic photosensitivity to the sun that enhances their mobility and ability to function. It also appears that vitamin D inhibits B cell proliferations and blocks B cell differentiation, as well as immunoglobulin secretion. Additionally, vitamin D from sun exposure suppresses T cell proliferation and results in a shift from a Th1 to a Th2 phenotype. This mechanism also affects T cell maturation and facilitates the induction of T regulatory cells, skewing away from the inflammatory Th17 phenotype. The direct result of these processes is a decreased production of inflammatory cytokines (IL-17, IL-21) with increased production of anti-inflammatory cytokines such as IL-10. Vitamin D also appears to have an effect on monocytes and dendritic cells, by inhibiting the production of inflammatory cytokines (IL-1, IL-6, IL-8, IL-12 and TNFα). By inhibiting DC differentiation and maturation, vitamin D also helps to preserve an immature phenotype. This is evidenced by a decreased expression of MHC class II molecules, co-stimulatory molecules and IL12.
The exciting field of research dubbed “photoimmunology” will inevitably continue to explore the profound relationship between sunlight and immunology, but what is already abundantly clear is that the sun does indeed play an intricate role in the optimal functioning and delicate balance of the immune system.
Patients at the Jewish Consumptives’ Relief Society (circa 1930) participated in heliotherapy, or sun exposure, as treatment for tuberculosis. Photo courtesy of Beck Archives, University of Denver.
Melatonin & Circadian Rhythm
Electronically published by the Brain Treatment Center of Asia ("Circadian Rhythm").
From an evolutionary perspective, your body has created a set of circadian rhythms that ebb and flow with the rise and setting of the sun. It’s your internal 24 hour clock. And unsurprisingly, bodily functions evolved to correspond with that rhythm. Light entering the eyes stimulates photoreceptors in rods, cones, and melanopsin-expressing retinal ganglion cells, which convert light signals to electric signals in the ganglion cells (absorption of energy). These cells then communicate photic input along the optic nerve to the hypothalamus, which controls your circadian rhythm. As light enters your body, the hypothalamus subsequently regulates melatonin, the body’s main sleep hormone. This operation stems from a group of about 20,000 neurons that form a structure called the suprachiasmatic nucleus (SCN). When natural blue light enters your eyes, like in the morning, the SCN decreases melatonin production. As light exposure decreases and becomes more red, like when the sun sets, the SCN increases melatonin production, making you tired. You can think of melatonin as your body’s signal that synchronizes your internal clock. It even plays a role in mitochondrial repair and individual peripheral clocks inside each cell. Interestingly, melatonin also enhances innate immunity, while sunlight exposure directly activates T-cells, as previously mentioned. Conversely, too much artificial blue light, like your TV, phone, or computer, can lower your innate immune response and increase your blood sugar levels.
If you lay in your bed reading from your cell phone or watching TV at nighttime, your body will absorb that light frequency and react accordingly, thinking that it’s morning. In fact, a study published in the Endocrine Society's Journal of Clinical Endocrinology & Metabolism found that exposure to a light source during the night, even something as simple as a street lamp outside your window, suppressed melatonin by around 85%. Another study by the University of Toronto found that those who wore glasses that block blue light wavelengths produced higher levels of melatonin than those who didn't during night shifts. Other studies even found that blue wavelengths specifically suppress delta brainwaves, which help to induce sleep, and instead boosts alpha wavelengths in order to create alertness.
Neuroscientist Andrew Huberman PhD of Stanford University notes that this is especially salient with blue light between the hours of 11:00 PM to 4:00 AM. He goes on to explain that bright light triggers pro-depressive circuits through the habenula, a structure in the thalamus. The habenula also connects to the pancreas through a specific pathway and because of this, bright lights can actually even alter blood sugar rhythms. Bright light, specifically bright blue light increases blood sugar and decreases insulin sensitivity. Since there is a circadian rhythm to the sensitivity of your eyes and skin to light, Huberman says that it might not even matter which frequency of light you’re absorbing, but that all bright light during these especially sensitive circadian hours will still increase blood sugar. UV light also naturally lowers your body’s adrenaline production and causes a cortisol release, which is the body’s stress hormone. It does this by allowing water flows to occur in the brain between glial cells and neurons via the aquaporin 4 gates. This process occurs around 4:00 AM and is nature’s way of waking up the human body.
According to a 2019 study published by the Society for the Study of Ingestive Behavior, negative blue light exposure interrupted the body’s ability to process sugar and its ability to regulate the body’s blood sugar with insulin. Thus, the researchers concluded that toxic blue light exposure may even lead to obesity or diabetes. Light is just as important, if not more important, than nutrition because even if your diet is absolutely perfect, negative light exposure can inhibit your body’s ability to process that food.
What About Vitamin D Supplements?
To put it bluntly, synthetic vitamin D supplements are not the same as natural synthesis from the sun. Sunlight creates close to 1,000 photochemicals in your plasma and active forms of vitamin D3, whereas supplementation will only give you an active form of vitamin D2. Excessive supplementation can also uncouple your endogenous system’s ability to naturally make D3. Incidentally, you can get vitamin D toxicity from synthetic pills, whereas you cannot reach a toxic level from sunlight due to the body’s natural mechanisms of prevention. Studies have also shown that vitamin D derived from sunlight has a much greater effect on bone calcification and homeostasis than supplementation groups.
The Natural Forms of Vitamin D
Vitamin D1 is a molecular compound of ergocalciferol (D2) with lumisterol in a 1:1 ratio.
Vitamin D2 (ergocalciferol) is produced by invertebrates, some plants, and fungi. Biological production of D2 is stimulated by ultraviolet light.
Vitamin D3 (cholecalciferol) is synthesized in the skin by the reaction of 7-dehydrocholesterol with UVB radiation, present in sunlight with an UV index of three or more.
Vitamin D4 is an analog scientifically known as 22-dihydroergocalciferol.
Vitamin D5 (sitocalciferol) is an analog created from 7-dehydrositosterol.
The Synthetic Forms of Vitamin D
Maxacalcitol (22-oxacalcitriol or OCT) is the first analog found to have a wider therapeutic window than 1,25(OH)2D3.
Calcipotriol is derived from calcitriol which was first discovered during trials involving the use of vitamin D for treating osteoporosis.
Dihydrotachysterol (DHT) is a synthetic form of vitamin D that many consider superior to natural D2 and D3. It becomes active by the liver without needing to go through hydroxylation in the kidneys.
Paricalcitol (19-norD2) is also derived from calcitriol. It is the first of the new vitamin D analogs to be approved for secondary hyperparathyroidism and differs from calcitriol in that it lacks the exocyclic carbon 19 and has a vitamin D2 side chain instead of a vitamin D3 side chain.
Tacalcitol is a derivative of vitamin D3. It is known to hinder keratinocytes in the skin.
Doxercalciferol (1α(OH)D2) is a prodrug and must be activated in vivo. It is less toxic than 1α (OH)D3 when administered chronically.
Falecalcitriol (1,25(OH) 2-26, 27-F6-D3) is approved for secondary hyperparathyroidism in Japan. It is more active than calcitriol because of its slower metabolism.
Rickets and the Discovery of Vitamin D
Dr. Theobald Palm
In the 1600’s, an industrial revolution swept through Europe. Buildings and houses were being built closer together in cities and coal was being burned causing unprecedented air pollution. At the same time, a bone deforming disease called rickets began appearing in children at alarming rates. The first scientist to theorize about the connection between the industrialization of Europe and the prevalence of rickets was a Polish man named Jędrzej Śniadecki in 1822. Śniadecki noticed that children that lived in inner city Warsaw had significantly higher rates of rickets than those that lived in the countryside.
In the 1880’s, Scottish doctor and missionary, Theobald Palm developed a very intelligent theory correlating sunlight exposure with risk of developing rickets. He studied an epidemiologic map of the prevalence of rickets published by the Collective Investigation Committee of the British Medical Association in 1889 and noticed that the disease was common in “large towns and thickly peopled districts.” During his previous travels to Tokyo and other areas closer to the equator, Palm had not seen rickets in the numbers that they were in the United Kingdom. However, his observations were largely ignored by the scientific and medical communities. Palm then went on to build his life’s work on his idea of “sunshine as a means of health.”
Nearly 100 years after Śniadecki’s initial observation, German pediatrician Kurt Huldschinsky would report to the scientific community that children exposed to a mercury arc lamp had dramatic improvement of their rickets within months. Huldschinsky was the first doctor to correctly realize that something was being made in the skin that impacted bone health and development in children.
Finally in 1921, two physicians named Alfred F. Hess and Lester J. Unger published the first ever case in a scientific journal where they cured rickets in children by exposing them to sunlight on the roof of their hospital in New York City. They also intelligently observed that children of color had significantly higher rates of rickets and required more time in the sun on the roof in order to obtain the same therapeutic outcome.
Around the same time, Harry Steenbock and Archie Black were experimenting with exposing various foods to light in order to see if that had any impact on rickets. They decided on using milk. This led to the addition of a fungal sterol called ergosterol to milk followed by UVB light exposure in order to add vitamin D2 to the milk. By 1931, this became common practice in the dairy industry in the United States and the United Kingdom. The US Government even implemented guidance to drink milk in order to develop strong bones. Within a few years, this practice essentially eradicated rickets.
Figure 5. from Sunlight and Vitamin D
Photographs of researchers who made crucial contributions to vitamin D and rickets research. (A) Jędrzej Śniadecki, (B) Kurt Huldschinsky, (C) Alfred Hess, (D) Harry Steenbock. Holick, copyright 2013. Reproduced with permission.
However, things got a bit out of hand in the 1940’s as many food products began implementing this vitamin D strategy to help market their foods as healthy. By the 1950’s, the extreme amount of vitamin D fortified food products on the market led to an outbreak of hypercalcemia in infants (children born with elfin-shaped faces, heart problems, and mental retardation), which an investigation by the Royal College of Physicians ruled to be caused by vitamin D toxicity. After that, many countries began reevaluating which foods were allowed to be vitamin D fortified and which were not. Today, milk and many juices are still vitamin D fortified in the US and Europe, but it begs the question: why not just recommend adequate sun exposure?
Figure 6. from Sunlight and Vitamin D
UV radiation therapy for rickets. (A) Photograph from the 1920s of a child with rickets being exposed to UV radiation. (B) Radiographs demonstrating florid rickets of the hand and wrist (left) and the same wrist and hand taken after treatment with 1 h UV radiation 2 times a week for 8 weeks. Note mineralization of the carpal bones and epiphyseal plates (right). Holick, copyright 2006. Reproduced with permission.
Figure 7. from Sunlight and Vitamin D
(A) Seal of a milk bottle that denoted that the milk was irradiated with UV radiation and contained vitamin D. (B) Cap of a milk bottle stating that activated ergosterol has been added to the milk. (C) Cap of milk bottle stating that the milk had been fortified with vitamin D. (D) Seal of a bottle of milk that denoted that the milk had been irradiated and contained vitamin D. Holick, copyright 2013. Reproduced with permission.
Figure 9. from Sunlight and Vitamin D
(A) Seal denoting that this product was fortified with vitamin D. (B) Bottle of oil denoting that it contained irradiated ergosterol. (C) Beer can denoting that it was fortified with vitamin D. (D) Advertisement denoting that Bird’s custard contained vitamin D. Holick, copyright 2013. Reproduced with permission.
The Rarely Seen History of Light Therapy
Niels Ryberg Finsen, December 15, 1860, Thorshavn, Faroe Islands; + 24 September 1904; Nobel Prize was awarded “in recognition of his contribution to the treatment of diseases, especially lupus vulgaris, with concentrated light radiation, whereby he has opened a new avenue for medical science.”
The first therapeutic uses of light date back to the end of the twentieth century, when a Danish researcher, Niels Ryberg Finsen, first showed that light helped to stimulate the immune system to fight infections. His artificial light was dubbed “the Finsen lamp.”
Light treatment had two branches: heliotherapy (natural sun therapy) and phototherapy (artificial light therapy). Heliotherapy was used to treat a wide variety of chronic illnesses in the early 1900’s, including tuberculosis and lupus, and it is still practiced in various parts of the world and especially in very northern latitudes.
Heliotherapy was particularly popular in Europe from around the turn of the century until the late 1930’s. One of its earliest practitioners was Dr. Auguste Rollier, who established a famous sun-therapy clinic in Leysin in the Swiss Alps. He treated all sorts of patients with varying diseases, who would be wheeled out onto a large sundeck for specific periods each day. However, the rise in the use of pharmaceutical drugs led to the demise of heliotherapy and therapeutic light recommendations over the last 100 years, especially in United States.
In the 1930’s, Charing Cross Hospital in London begin regularly using “sun-lamps” in order to treat circulatory diseases, anaemia, varicose veins, heart disease and degenerative disorders.
In the early 1940’s in the United States, Emmitt Knott developed his most famous invention: the “Knott Hemo-Irradiator.” Knott found that irradiation of just 50±100cc of blood with ultra-violet light, followed by a transfusion back into the patient was effective in the treatment of puerperal sepsis, peritonitis, encephalitis, polio, and herpes simplex. By 1947, upwards of 80,000 patients had been treated with the Knott Hemo-Irradiator,” with reported success rates of 50-80%. This device later came under intense scrutiny as we now know that prolonged radiation exposure can increase the risk of cancer.
However, new versions of Knott’s original invention, namely intravenous laser blood irradiation have begun to make a come back and can be found in many clinics around the world. Recent studies have yielded promising results and are helping to elucidate the safety around this modern therapy.
However, more studies are needed to ascertain the appropriate protocols and applications of this technology.
Intravenous Laser Therapy being performed by The New York Center for Innovative Medicine (NYCIM).
Gallery of historical light therapies compliments of Rare Historical Photos.
The Modern World
Between 1850-1860, English chemist Joseph Swan was working on an invention. He was developing the world’s first light bulb by using canonized paper filaments. In 1878, he was issued a patent on his invention in the United Kingdom. The world turned its head to see what the fuss of this new invention was all about. Among them was an American named Thomas Edison.
Edison closely examined the new invention, but saw a major flaw with it: a thinner filament with higher electrical resistance would require less electricity to glow. In 1879, one year after Swan had shown his new invention to the world, Edison won the U.S. and Canadian patents on the lightbulb. He founded the Edison Electric Illuminating Company of New York in 1880, decidedly using a carbonized bamboo filament in his light bulbs because it was capable of burning for more than 1,200 hours.
Until this moment, throughout all of human history, our only light exposure was direct sunlight or candlelight/fire.
General Electric then helped slingshot the advancement of light bulbs over the next century; first with a physicist named William David Coolidge, who began using tungsten filaments, and then later Nick Holonyak, who accidentally invented the red LED light for the company while trying to create a laser. Subsequently, yellow and green LEDs were added to the mix and then eventually the blue LED, created in the early 1990’s by Isamu Akasaki, Hiroshi Amano, and Shuji Nakamura, a group of Japanese and American scientists, for which they won the 2014 Nobel Prize in Physics. It only took a little more than 100 years and humans went from only natural sunlight to blue LED lights being used everyday. It happened so fast that one has to ask: are there any long term health implications stemming from this new found control over our light sources?
Sir William Crookes - 1906
In nature, the sun emits the entire light spectrum during the daytime, each frequency doing something different to the human body. Think of blue light as a powerful stimulant, whereas red light is more calming and regenerative. The red light counteracts the natural blue light emitted from the sun without hurting you, each playing their parts in a delicate dance between nature and your mitochondria. But as you may even be reading this on one of your electrical devices, most modern inventions, TVs, smartphones, computers, etc, only utilize blue light sources. Why do we only use blue light in these devices, you may be asking. It’s significantly cheaper to subtract other frequencies, like red light. Blue light “wastes” less energy and saves more money. Artificial light manufacturers have made decisions about the light sources you use everyday based on cost, not biology.
Ok, we’ve talked about man made sources of light, but what about man made tools to block light? Let’s look at sunglasses for example. Sunglasses are, after all, a very modern invention. In 1913, a British chemist named Sir William Crookes introduced his spectacle lenses containing cerium, which blocked UV light. They were originally created to be prescribed to patients with syphilis, as extreme light sensitivity was a common symptom of the disease. However, after a while, an American businessman named Sam Foster began mass producing inexpensive “sunglasses'' in 1929, helping to cement the item as an accessory in American fashion. In 1938, Life magazine elaborated that sunglasses were a "new fad for wear on city streets ... a favorite affectation of thousands of women all over the U.S.''
Sunglasses seem to operate as a weird crossroads between fashion and misguided science, where medical professionals urge you to wear them in order to protect your eyes and fashion brands design styles that are the “must-haves” of each season. It’s a perfect storm for American consumerism.
However, there may be a cost to our modern use of sunglasses. In his book, Health and Light, Dr. John Ott talks about possible carcinogenic effects from filtering natural light through sunglasses. This was most notable in the work of Dr. Albert Schweitzer, who observed the rate of cancer in Lambarene on the west coast of Africa. When Dr. Schweitzer started the local hospital, there was no cancer at all in the community, but suddenly cancer cases took an uptick. The only difference that the doctor observed is that the native people had started wearing sunglasses to symbolize the status that came with a civilized world. His hypothesis was that by introducing sunglasses to the native people in this village, many cancers came with it due to the lack of the normal sunlight exposure that the people had in their retinas.
To further this theory, researchers published a study in JAMA Neurol on the Association of Retinal Nerve Fiber Layer Thinning With Current and Future Cognitive Decline. The study examined more than 500,000 UK residents between the age of 40 and 69 and measured the thickness of their retinal nerve fiber in order to compare it to cognitive testing. The authors outline how blue light exposure thins your retina because of the melanopsin/retinal mechanism. Sunglasses increase that same risk. Those in the study with a thinner RNFL were twice as likely to experience cognitive decline within 3 years. If you wear sunglasses during the day and absorb blue light from your phone or TV in the evening, then you are significantly increasing your risk of neurodegeneration.
A similar mechanism can be observed with modern sunscreens. In his book, 2000 Years of Zinc and Brass, Paul T. Craddock, the head of Metal Research in the Department of Scientific Research at the British Museum, notes that zinc may have been one of the earliest primitive forms of sunscreen as historical contents shows both the Indians in 500 BC, as well as the Greeks, both using zinc oxide as a medical salve for skin cancers. There are even accounts of nomadic sea-populations in the Philippines, Malaysia, and Indonesia using a paste of tree bark to help prevent their skin from burning during long days at sea.
Modern sunscreen, however, wasn't used until 1928. Originally brought to market by French chemist, Eugène Schueller, the founder of L’Oreal, sunscreens weren’t a very popular beauty item when they launched. It wasn’t until 1944 when an airman and pharmacist, named Benjamin Green, created a sunscreen for the U.S. military to protect soldiers in the tropics during WWII that sunscreen took off. Brands like Coppertone, back in the U.S., saw an opportunity to bring a new product to market. They improved the consistency and commercialized the idea of sunscreen under the famous Coppertone girl branding, which advertised a cream to help darken the appearance of your tan. Suddenly, women all across the country wanted sunscreen for the beach, for tanning, and for time in the sun. Commercial sunscreen was created as a beauty product, not out of medical necessity. Eventually, brands would introduce water-resistance sunscreens and longer-lasting, broader-spectrum variations - all adding toxic chemicals to our skin and blocking our main synthesis of vitamin D.
Sunscreen use is a hallmark of public health campaigns for skin cancer prevention, but many epidemiological studies have recently questioned that claim altogether. In a systematic review and meta-analysis to assess this association, researchers closely examined 29 previous studies, involving 313,717 participants. The meta-analysis showed no correlation between sunscreen and skin cancer. Other studies have shown that sunscreen can significantly decrease vitamin D production in the body, which is a common presentation in case studies of individuals that had developed cancer.
It’s worth noting that most of the sunscreens contain toxic chemicals that may be harmful for you and should be avoided altogether. Scientists at the Environmental Working Group (EWG), a national environmental organization that analyzes toxic chemical use in consumer products, found that only 21% of sunscreens on the market were found to be below their toxic threshold. Many sunscreens on the market have even been studied and found to have a neurotoxic effect. So what should you use to protect your skin? A good form of sunscreen is zinc oxide and/or titanium dioxide and antioxidants. However, a research team at Oregon State University noted that when zinc oxide is mixed with other common ingredients in sunscreens, it can become toxic under ultraviolet radiation. So, it’s important to make sure your sunscreen only contains zinc oxide and no other additives. You definitely want to avoid toxic ingredients such as parsol 1789, avobenzone, mexoryl, oxybenzone, retinyl palmitate, or helioplex.
Interestingly, Astaxanthin is a red carotenoid found in shrimp, crab, salmon and microalgae, which has also shown protective properties from the sun when supplemented because of its strong anti-oxidative properties. Other antioxidant-risk foods that can be helpful if you’re spending time in the sun include omega-3’s, resveratrol, catechizes, vitamin E, and beta-carotene. It’s also a good idea to use clothing with long sleeves or hats if you have a long day of sun exposure, making sure that the weave in your clothing is tight enough to block harmful UV rays.
Sunburns & Skin Cancer
What about sunburn then? Shouldn’t we prevent burns from happening in order to prevent skin cancer?
Types of skin cancer, compliments of the Mayo Clinic.
A sunburn is not a thermal burn, as most people think it is, meaning that it is not due to direct heat from the sun. There are cells in the epidermis called keratinocytes, which are responsible for producing keratin. In order to exert a biological response, such as the conversation of 7-dehydrocholesterol to previtamin D, the UVB rays need to be absorbed by a cellular chromophore. This transduces the light energy into a biochemical signal. Genomic DNA is the major chromophore for UVB and for most of the common photoproducts that are also produced. However, sometimes a very strong dosage of UVB rays can damage the DNA or other chromophores in the keratinocytes. When that damage becomes so severe that it is irreversible, these skin cells must go through a programmed cell death called apoptosis. The red appearance and painful feelings associated with sunburns are due to inflammation and vasodilation caused by the UVB exposure and this genomic cell death process. There is a very intricate balance between cell survival and apoptogenic factors which determines the cell’s final fate. Growing evidence suggests that skin cancer is caused by the deregulation of this balance due to chronic UVB stress, particularly when that UVB stress causes alterations in the p53 tumor suppressor gene. The p53 gene is sometimes called the “guardian of the genome” because it is responsible for aiding DNA repair or causing the elimination of cells with irreversible DNA damage. When the p53 gene becomes damaged, cells that should die instead stay alive and replicate their already severely damaged DNA into cancerous cells (carcinogenesis). Several studies have shown that UV induces unique types of p53 mutations causing skin cancers at rates that are not found in other types of human cancer. In addition to the p53 gene, other tumor suppressor genes have been implicated in different skin cancers, such as the relationship between the patched (ptc) gene and nevoid basal cell carcinoma syndrome (NBCCS). Rates of skin cancer have been rapiding increasing over the past 50 years and scientists have been posing many different theories as to why. Some have suggested that holes in the ozone layer have caused a never before seen increase in UVB exposure, while others have suggested that our lifestyle changes may be the cause.
The scientific body of literature on moderate to high sun exposure is growing rapidly, but melanoma and its relationship to sun exposure is not adequately addressed in the current literature. A 2016 review of “The risks and benefits of sun exposure” helps to elucidate this complex topic, but the intricate details still remain a mystery. To confuse things even more, some researchers have suggested that vitamin D may actually have a protective effect against skin cancers, but the results from investigations have been altogether inconclusive and conflicting. It seems to me that the current medical recommendations may be too avoidant of the sun and perhaps future research should focus on tools to prevent DNA damage from the sun without limiting exposure that would trigger optimal vitamin D production. Nonetheless, one glaring question remains unanswered:
If the use of sun-protective tools, such as sunscreens, sunglasses, and sun-avoidance, has been continually increasing worldwide for the last 100 years, then why has the prevalence of sun exposure-related pathologies and skin cancers also been on the rise?
Photo of the four main types of skin cancers, from SurgMedia.
It’s worth noting that other research has indicated that fasting, or calorie restriction diets such as intermittent fasting, can have protective effects against skin cancer by encouraging apoptosis (cell death) and modulating certain epithelial growth factors that may help to prevent cancer. One could theorize that ancient humans would have obviously included fasting in their diets more than modern man because of the nature of hunting and food scarcity. It wouldn’t take much of a leap to suggest that fasting, combined with a radiation hormesis effect, could have potentially provided our ancestors with a better natural protection from the sun than we have today. However, more studies will need to be done to investigate this relationship.
Avoiding sugar can also help to decrease risk of sun damage. Sugar contributes to the formation of advanced glycation end-products (AGE’s), which speeds up the aging process of vascular and connective tissues. Some studies have suggested that UV radiation may be more harmful to the skin, when the skin tissue has an excessive build up of AGE’s due to sugar consumption. Other research has found that proanthocyanidins can protect DNA from mutation, which includes protection from UV radiation.
In ancient Egypt, kings and queens were regarded as offspring and sometimes even the incarnation of the sun.
While there are many unknowns when it comes to light, it remains abundantly clear that it remains crucially important to our biology and provides a life-giving force. It’s no coincidence that humans have worshipped and honored the sun for most of human history. In the pre-Columbian civilizations of Mexico and Peru, sun worship was a prominent center of their culture. In Aztec religion, extensive human sacrifice was offered to the sun gods Huitzilopochtli and Tezcatlipoca. In both Mexican and Peruvian ancient religions, the Sun occupied a central fixture in both myth and ritual. The Egyptians honored the sun god, Ra. In many Native American cultures, such as the Iroquois and Plains peoples, the sun was recognized as a life-giving force and they performed a yearly sun dance. The Greeks honored Helios, whom Homer described as “giving light both to gods and men.” Hindus worshipped the Sun God Surya, who was believed to be able to heal the sick. Sun worship has also been found in Persian societies, Babylonian texts, and in many Asian religions. Christian tradition pays specific attention to the sun throughout its text, most notably in the creation story in Genesis when God said, “Let there be light: and there was light.”
And God said, Let there be lights in the firmament of the heaven to divide the day from the night; and let them be for signs, and for seasons, and for days, and years: And let them be for lights in the firmament of the heaven to give light upon the earth: and it was so.
And God made two great lights; the greater light to rule the day, and the lesser light to rule the night: he made the stars also. And God set them in the firmament of the heaven to give light upon the earth: and it was so.
Seemingly, we may be one of the only civilizations in human history that have forgotten how important sunlight really is to our existence…
…perhaps it’s time we remembered.
A representation of the Incan Sun deity.